Intestinal Dysbiosis Gut Imbalance: Sibo Explained
The human gut is a complex ecosystem, home to trillions of microorganisms that play a critical role in maintaining our overall health. When this ecosystem is in balance, it aids in digestion, nutrient absorption, immune function, and more. However, when an imbalance occurs, it can lead to a condition known as Small Intestinal Bacterial Overgrowth (SIBO), which can have significant health implications.
This glossary article aims to provide a comprehensive understanding of the concept of intestinal dysbiosis, its relationship with SIBO, and the various aspects related to it. The information presented here is based on extensive research and is intended to serve as a reliable resource for those seeking to understand these complex topics in depth.
Understanding the Gut Microbiome
The gut microbiome refers to the community of microorganisms, including bacteria, viruses, fungi, and other microbes, that reside in our digestive tract. These organisms are not merely passengers; they play a vital role in our health and wellbeing. They help in digesting food, producing essential vitamins, training our immune system, and even influencing our mood and behavior.
However, the gut microbiome is a delicate ecosystem that can be easily disrupted by factors such as diet, stress, lack of sleep, and the use of certain medications, particularly antibiotics. When this disruption occurs, it can lead to a condition known as dysbiosis, which is characterized by an imbalance in the composition of the gut microbiota.
Role of Gut Microbiome in Health
The gut microbiome plays a crucial role in maintaining our health. It aids in the digestion of food, particularly the breakdown of complex carbohydrates, and the absorption of nutrients. It also produces essential vitamins such as vitamin K and certain B vitamins. Moreover, it plays a critical role in training our immune system and protecting us from harmful pathogens.
Research has also shown that the gut microbiome can influence our mood and behavior. This is often referred to as the gut-brain axis, a bidirectional communication system between the gut and the brain. Dysregulation of this axis has been linked to various mental health conditions, including depression and anxiety.
Factors Affecting the Gut Microbiome
Several factors can influence the composition and function of the gut microbiome. These include diet, stress, sleep, physical activity, and the use of certain medications. A diet high in processed foods and low in fiber, for example, can lead to a decrease in the diversity of the gut microbiota, which is associated with poor health.
Stress and lack of sleep can also negatively impact the gut microbiome. Chronic stress has been shown to alter the composition of the gut microbiota, while lack of sleep can disrupt the normal circadian rhythms of the gut microbes. Physical activity, on the other hand, has been shown to have a positive effect on the gut microbiome, increasing its diversity and function.
Understanding Intestinal Dysbiosis
Intestinal dysbiosis refers to an imbalance in the composition of the gut microbiota. This can occur when there is an overgrowth of harmful bacteria or a decrease in beneficial bacteria. Dysbiosis can lead to a variety of health problems, including digestive issues, immune dysfunction, and increased risk of chronic diseases.
It's important to note that dysbiosis is not a disease in itself, but rather a condition that can contribute to disease development. It's also not always clear whether dysbiosis is a cause or a consequence of disease, as this can vary depending on the specific condition.
Causes of Intestinal Dysbiosis
There are several potential causes of intestinal dysbiosis. These include poor diet, stress, lack of sleep, physical inactivity, and the use of certain medications, particularly antibiotics. Antibiotics can disrupt the gut microbiome by killing both harmful and beneficial bacteria, leading to an imbalance.
Other factors that can contribute to dysbiosis include aging, smoking, excessive alcohol consumption, and certain health conditions, such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and obesity. Genetic factors may also play a role, as research has shown that the composition of the gut microbiota can be influenced by our genes.
Health Consequences of Intestinal Dysbiosis
Intestinal dysbiosis can have a wide range of health consequences. It can lead to digestive issues, such as bloating, constipation, diarrhea, and abdominal pain. It can also contribute to immune dysfunction, as the gut microbiome plays a critical role in training our immune system and protecting us from harmful pathogens.
Research has also linked dysbiosis to an increased risk of chronic diseases, including obesity, type 2 diabetes, cardiovascular disease, and certain types of cancer. Moreover, dysbiosis has been associated with various mental health conditions, such as depression and anxiety, due to the role of the gut microbiome in the gut-brain axis.
Understanding Small Intestinal Bacterial Overgrowth (SIBO)
Small Intestinal Bacterial Overgrowth (SIBO) is a condition characterized by an excessive amount of bacteria in the small intestine. While the small intestine normally contains a relatively small number of bacteria compared to the large intestine, in SIBO, the bacterial population in the small intestine becomes significantly increased.
SIBO can lead to a variety of symptoms, including bloating, abdominal pain, diarrhea, constipation, and malabsorption of nutrients. If left untreated, it can lead to serious health complications, including vitamin and mineral deficiencies, malnutrition, and damage to the lining of the small intestine.
Causes of SIBO
There are several potential causes of SIBO. These include structural abnormalities in the small intestine, motility disorders that slow the movement of food and bacteria through the small intestine, and conditions that decrease the production of stomach acid, which helps to keep the bacterial population in the small intestine in check.
Other factors that can contribute to SIBO include the use of certain medications, particularly proton pump inhibitors (PPIs) and antibiotics, and certain health conditions, such as diabetes, scleroderma, and Crohn's disease. Aging may also increase the risk of SIBO, as older adults often have decreased motility and stomach acid production.
Diagnosis and Treatment of SIBO
SIBO is typically diagnosed through a breath test, which measures the levels of hydrogen and methane in the breath after the consumption of a sugar solution. These gases are produced by bacteria in the small intestine and can indicate an overgrowth. However, the breath test is not perfect and can sometimes yield false positive or negative results.
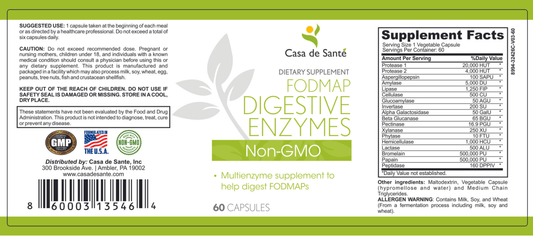
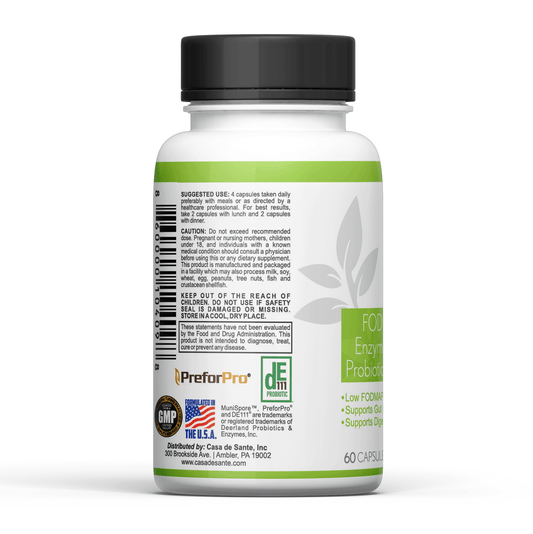
The treatment of SIBO typically involves the use of antibiotics to reduce the bacterial overgrowth. Dietary changes may also be recommended, such as a low-FODMAP diet, which limits the intake of certain types of carbohydrates that can be fermented by gut bacteria. In some cases, probiotics may be used to help restore the balance of the gut microbiota.
Connection Between Intestinal Dysbiosis and SIBO
Intestinal dysbiosis and SIBO are closely related, as both involve an imbalance in the gut microbiota. In fact, SIBO can be considered a form of dysbiosis, as it involves an overgrowth of bacteria in a specific part of the gut. However, while dysbiosis can occur anywhere in the gut, SIBO specifically refers to an overgrowth in the small intestine.
Both dysbiosis and SIBO can lead to similar symptoms, such as bloating, abdominal pain, and altered bowel habits. They can also both contribute to the development of various health conditions, including digestive disorders, immune dysfunction, and chronic diseases. Therefore, maintaining a healthy gut microbiome is crucial for preventing both dysbiosis and SIBO.
Preventing and Managing Dysbiosis and SIBO
There are several strategies for preventing and managing dysbiosis and SIBO. These include maintaining a healthy diet, managing stress, getting enough sleep, staying physically active, and using medications judiciously. A diet high in fiber and low in processed foods can help to maintain a healthy gut microbiome, while stress management and sleep can help to prevent disruptions to the gut microbiome.
When it comes to medications, it's important to use antibiotics only when necessary, as they can disrupt the gut microbiome and lead to dysbiosis. Proton pump inhibitors (PPIs) should also be used with caution, as they can decrease stomach acid production and increase the risk of SIBO. If you have a health condition that increases your risk of dysbiosis or SIBO, it's important to manage it effectively and work with your healthcare provider to monitor your gut health.
Role of Probiotics and Prebiotics
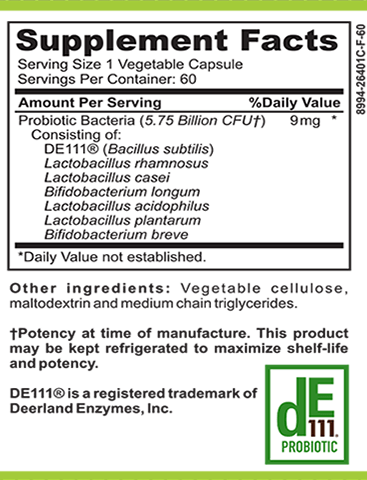
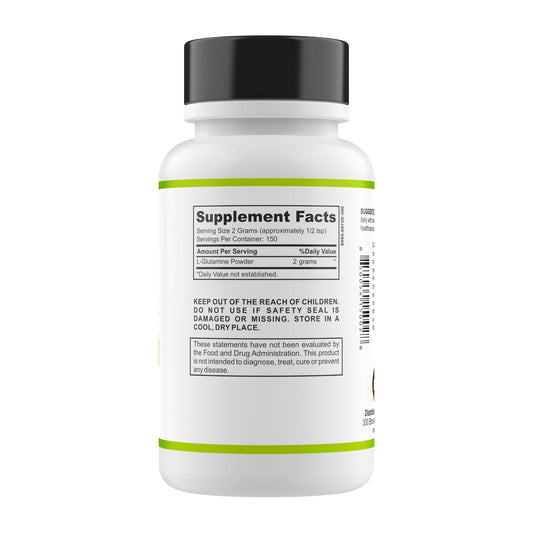
Probiotics and prebiotics can also play a role in preventing and managing dysbiosis and SIBO. Probiotics are live bacteria and yeasts that are beneficial for our gut health, while prebiotics are types of dietary fiber that feed the beneficial bacteria in our gut.
Research has shown that probiotics can help to restore the balance of the gut microbiota and alleviate symptoms of dysbiosis and SIBO. Prebiotics, on the other hand, can help to promote the growth of beneficial bacteria and enhance the health of the gut microbiome. However, it's important to note that not all probiotics and prebiotics are the same, and their effectiveness can vary depending on the specific strains and doses used.
Conclusion
Intestinal dysbiosis and SIBO are complex conditions that involve an imbalance in the gut microbiota. They can have significant health implications, contributing to a variety of symptoms and increasing the risk of various health conditions. However, with a better understanding of these conditions and the factors that influence our gut health, we can take steps to maintain a healthy gut microbiome and prevent dysbiosis and SIBO.
Remember, maintaining a healthy gut is not just about diet and lifestyle, but also about understanding the complex ecosystem within us and how it interacts with our body and our environment. By doing so, we can better appreciate the importance of our gut health and take proactive steps to nurture and protect it.